Vasectomy and Postoperative Complications: Prevention and Management
A vasectomy is one of the most effective and permanent methods of male contraception, chosen by millions of men worldwide. It offers a reliable, safe, and minimally invasive solution for those seeking long-term birth control. However, like any surgical procedure, vasectomy can be associated with postoperative complications. While most are minor and temporary, understanding their causes, prevention strategies, and treatment options is crucial for both patients and healthcare professionals.
This article provides a comprehensive, evidence-based overview of vasectomy and postoperative complications, emphasizing prevention and management approaches that enhance recovery and long-term outcomes.
Understanding Vasectomy: The Basics
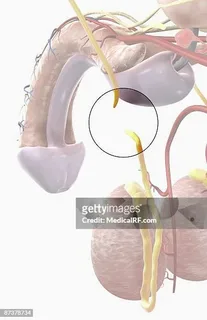
A vasectomy involves cutting or sealing the vas deferens — the tubes that carry sperm from the testicles to the urethra — to prevent sperm from mixing with semen. The procedure can be performed using traditional or no-scalpel vasectomy (NSV) techniques.
Both methods are outpatient procedures, typically lasting less than 30 minutes, with local anesthesia and minimal downtime. Despite this simplicity, some men experience short-term discomfort, swelling, or other postoperative complications that require medical attention.
Common Postoperative Complications After Vasectomy
Most complications following a vasectomy are mild, but understanding them in detail helps with prevention and prompt management. Below are the most frequently encountered postoperative issues:
1. Hematoma (Bleeding Under the Skin)
A hematoma is the collection of blood within the scrotal tissue, often caused by bleeding from small blood vessels during or after surgery.
Symptoms:
- Painful swelling or bruising of the scrotum
- Firm or tender mass under the incision
- Discoloration that worsens in the first few days
Prevention:
- Careful surgical technique to minimize vessel injury
- Adequate compression and rest post-surgery
- Avoiding physical exertion for at least 48 hours
Management:
Most hematomas resolve spontaneously within 1–2 weeks. Application of ice packs, scrotal support, and pain control with NSAIDs can ease discomfort. Large or expanding hematomas may require drainage by a urologist.
2. Infection
Postoperative infection is one of the most common vasectomy complications. It can occur at the incision site or within deeper scrotal tissue.
Symptoms:
- Redness and warmth around the incision
- Fever or chills
- Pus discharge or foul odor
- Increased tenderness or swelling
Prevention:
- Proper antiseptic preparation before surgery
- Use of sterile instruments and gloves
- Patient adherence to wound care instructions (keeping the area clean and dry)
Management:
Mild infections are treated with oral antibiotics and wound hygiene. In severe cases (e.g., abscess formation), surgical drainage may be necessary.
3. Sperm Granuloma
A sperm granuloma forms when sperm leak from the cut ends of the vas deferens, triggering an inflammatory immune response.
Symptoms:
- Small, firm lump near the surgical site
- Mild to moderate tenderness
- Occasionally radiating pain during ejaculation
Prevention:
- Sealing the vas deferens properly (e.g., cauterization or fascial interposition)
- Avoiding early ejaculation before the site has healed
Management:
Most granulomas resolve without intervention. Persistent or painful lumps may require anti-inflammatory medication or, in rare cases, surgical excision.
4. Epididymitis and Congestive Pain
Inflammation of the epididymis (the coiled tube behind the testicle that stores sperm) can develop when sperm backflow occurs after vasectomy.
Symptoms:
- Dull ache or heaviness in the testicles
- Localized swelling or tenderness
- Pain that increases after physical activity
Prevention:
- Gradual resumption of activity post-surgery
- Use of supportive underwear to reduce strain
Management:
Treatment typically includes anti-inflammatory medications, warm compresses, and rest. In persistent cases, antibiotics are prescribed if infection is suspected.
5. Post-Vasectomy Pain Syndrome (PVPS)
Post-Vasectomy Pain Syndrome refers to chronic scrotal or testicular pain lasting longer than three months after surgery. It occurs in about 1–2% of men, though mild discomfort is more common.
Symptoms:
- Persistent aching or sharp pain
- Pain during ejaculation or intercourse
- Discomfort during physical activity
Possible Causes:
- Nerve entrapment or damage
- Sperm congestion and pressure buildup
- Chronic inflammation or scarring
Prevention:
- Use of minimally invasive techniques (such as no-scalpel vasectomy)
- Gentle handling of tissue during surgery
Management:
- Conservative treatment with anti-inflammatory medications, heat therapy, and nerve blocks
- In severe cases, microsurgical reversal or epididymectomy may be required
6. Granulomatous Reactions and Autoimmune Response
Following vasectomy, sperm can enter the bloodstream, triggering an autoimmune reaction in some individuals. This can lead to inflammation or antibody production against sperm.
Prevention:
- Using sealing techniques that reduce sperm leakage
- Monitoring patients with autoimmune risk factors
Management:
- Usually self-limiting; however, corticosteroids or anti-inflammatory agents may be prescribed in symptomatic cases.
7. Swelling and Bruising
Mild swelling and bruising are normal after vasectomy, peaking within 48 hours. However, excessive swelling may indicate hematoma or infection.
Prevention:
- Ice application (20 minutes every 2–3 hours for the first 24 hours)
- Elevating the scrotum during rest
- Avoiding tight clothing
Management:
Most cases resolve spontaneously. Persistent or worsening swelling should be evaluated by a urologist.
8. Psychological Impact
While not a physical complication, psychological discomfort can arise due to anxiety, regret, or fear about fertility loss.
Prevention:
- Preoperative counseling to ensure informed decision-making
- Clear explanation of procedure permanence and options for future fertility
Management:
- Support from mental health professionals or counselors
- Open communication with the partner
Preventive Strategies for Post-Vasectomy Complications
Prevention begins before the first incision is made. Urologists and patients play equal roles in minimizing risks.
A. Surgeon-Level Prevention
- Aseptic Technique:
Strict adherence to sterile protocols reduces infection risk. - Minimally Invasive Approaches:
The no-scalpel vasectomy significantly reduces bleeding, infection, and recovery time. - Effective Sealing Methods:
Combining cauterization, clips, and fascial interposition minimizes sperm leakage and granuloma formation. - Patient Selection:
Screening for bleeding disorders, diabetes, or immunosuppression ensures safer outcomes.
B. Patient-Level Prevention
- Follow Postoperative Instructions Carefully:
Avoid heavy lifting, sexual activity, or strenuous exercise for at least a week. - Wound Hygiene:
Keep the incision clean and dry; avoid soaking in baths for the first 48 hours. - Scrotal Support:
Wearing snug briefs or a jockstrap reduces tension and swelling. - Cold Compresses:
Ice therapy minimizes pain and inflammation in the early phase. - Monitor for Warning Signs:
Promptly report fever, severe pain, or abnormal discharge to the healthcare provider.
Management Approaches for Common Complications
Once complications occur, management should be swift, evidence-based, and tailored to severity.
1. Pain and Swelling
- Use of NSAIDs (e.g., ibuprofen or naproxen)
- Ice packs and rest
- Supportive underwear
2. Infection
- Oral or intravenous antibiotics
- Incision drainage if abscess develops
- Maintaining proper hygiene
3. Chronic Pain
- Nerve blocks or local anesthetic injections
- Physiotherapy and scrotal massage
- In refractory cases, microsurgical reversal or denervation
4. Sperm Granuloma
- Observation for mild cases
- Anti-inflammatory medications
- Surgical excision if painful or persistent
5. Psychological Support
- Pre- and post-operative counseling
- Education about normal healing patterns
Role of the No-Scalpel Vasectomy in Reducing Complications
The no-scalpel vasectomy (NSV), introduced in China and now widely used worldwide, offers a less invasive approach.
Key Advantages:
- Reduced bleeding and infection rates
- Minimal tissue trauma
- Shorter recovery period
- Lower risk of chronic pain
Mechanism:
Instead of incising the scrotum, the surgeon punctures the skin to access the vas deferens. This simple difference dramatically lowers postoperative complication rates.
Long-Term Outlook After Vasectomy
Most men recover within 1–2 weeks without any major issues. Chronic complications are rare and usually manageable. Studies show that over 95% of men report satisfaction with their vasectomy outcomes when proper preventive care and postoperative management are followed.
The long-term outlook remains excellent — vasectomy does not affect testosterone production, libido, or erectile function. The key lies in awareness, early intervention, and open communication with healthcare providers.
Key Takeaways
- Vasectomy is a safe and permanent birth control option with a very low complication rate.
- Most postoperative complications are minor, temporary, and preventable with proper care.
- Early management of pain, infection, or inflammation leads to faster recovery and better outcomes.
- The no-scalpel vasectomy technique offers superior safety and minimal downtime.
- Ongoing communication between patient and physician ensures optimal recovery and mental reassurance.
FAQs About Vasectomy and Postoperative Complications
1. How common are complications after vasectomy?
Complications are rare. Minor issues like swelling, bruising, or mild pain occur in about 5–10% of men and usually resolve within a few days. Serious complications such as infection or chronic pain affect less than 2%.
2. What can I do to prevent infection after vasectomy?
Keep the surgical area clean and dry for the first 48 hours. Avoid swimming, sexual activity, and exercise during this time. Follow your urologist’s wound care instructions closely, and report any redness or discharge immediately.
3. When should I call my doctor after a vasectomy?
Contact your doctor if you experience fever, severe pain, excessive swelling, or pus-like discharge. Persistent discomfort lasting more than two weeks should also be evaluated to rule out infection, granuloma, or nerve irritation.
In summary, vasectomy remains one of the most reliable forms of contraception available to men today. Understanding vasectomy and postoperative complications, and applying evidence-based prevention and management strategies, ensures that patients experience a safe procedure and a smooth recovery — reaffirming the vasectomy’s position as a cornerstone of responsible family planning.